Research efforts on diseases of the human eye and neural function are hampered by the fact that these organs degrade rapidly after death. In addition, the eyes of animals are still different from ours. To remedy this, an international team of researchers has developed a new method to “bring back to life” retinas taken from donors, 5 hours after their death. This technical feat will allow new studies on the functioning of the human eye, the nervous system, but also concerning the extension of the lifespan of the organs to be transplanted. This success also offers new perspectives for the treatment of neurodegenerative diseases, including age-related macular degeneration.
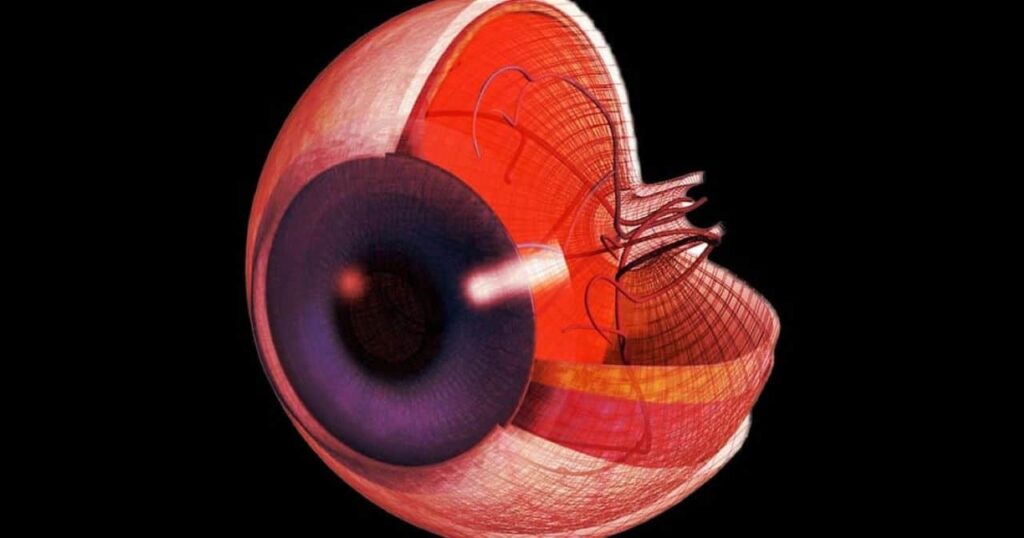
Death is defined as the irreversible arrest of circulatory, respiratory or cerebral activity. Many peripheral human organs can be transplanted from deceased donors using protocols to optimize viability. However, tissues of the central nervous system and some associated organs, such as the eyes, rapidly lose their viability after the circulation stops, hampering their potential for transplantation. Indeed, billions of neurons in the central nervous system transmit sensory information in the form of electrical signals; in the eye, specialized neurons called photoreceptors detect light. These cells die quickly after the heart stops. Nevertheless, the time course and mechanisms causing neuronal death, as well as the potential for reactivation, remain poorly defined.
In order to better understand how nerve cells succumb to a lack of oxygen induced by the cessation of general circulatory activity, a team of American and Swiss researchers used the retina as a model of the central nervous system. They measured the activity of murine (mouse) and human retinal cells shortly after death, and developed new methods to bring them back to life. Their work is published in the journal Nature.
Restoring cellular communication after death
To achieve their goal, Scripps Research Associate Professor Anne Hanneken was able to provide more than 40 eyes from organ donors, within 20 minutes of death. Frans Vinberg of the Moran Eye Center, meanwhile, designed a special transport unit to restore oxygenation and other nutrients to donor eyes, as well as a device to stimulate the retina and measure the electrical activity of his cells. The team therefore proceeded in two stages.
First, the researchers demonstrated the rapid decline of neuronal signaling and identified the conditions necessary for the potential resuscitation of eye cells live in mice, after death, and in the human retina. Secondly, they measured the responses induced by light in the human macular photoreceptors of the eyes, taken from the donors, up to 5 hours after their death. They were then able to identify modifiable factors leading to reversible and irreversible loss of light signaling after death.
While early experiments revived the photoreceptors, the cells seemed to have lost their ability to communicate with other cells in the retina. The team identified oxygen deprivation as the critical factor leading to this loss of communication.
Fatima Abbas, of the Moran Eye Center and lead author of the study, explains in a press release: We were able to awaken photoreceptor cells in the human macula, which is the part of the retina responsible for our central vision and our ability to see fine detail and color. In eyes obtained up to five hours after the death of an organ donor, these cells responded to bright light, colored lights, and even very faint flashes of light. « .
Using their innovative approach to keep cells oxygenated for longer periods of time—lengthening the time the retina and neuronal cells can survive—the team was able to restore a specific electrical signal seen in living eyes, « the wave b”. The latter testifies to a communication between all the layers of macular cells that allow us to see. This is the first recording post mortem b wave, directed from the center of a human retina. However, this temporary return of retinal cell activity does not mean that the donor eyeballs could « see ». Higher visual centers in the brain are needed to revive the whole process of seeing.
Frans Vinberg says: “ We were able to get retinal cells to communicate, as they do in the living eye to mediate human vision. Previous studies have restored very limited electrical activity in the eyes of organ donors, but this has never been achieved in the macula, and never to the extent that we have now demonstrated. « .
In view of these results, some experts question the irreversible nature of death in the central nervous system. Indeed, if it is possible to preserve certain organs of the human body for a transplant, the central nervous system ceases to function far too quickly for it to be “recovered”, in the perspective of a transplant. Nevertheless, all the constituent elements of our nervous system do not die at the same speed, “survival” mechanisms are sometimes established for some time, the concept of death is then more complex. In this context, the feats described in the article would make it possible to see things more clearly (no pun intended) and to indicate new possibilities in terms of medical advances.
Study neurodegenerative diseases
The process demonstrated by the team could therefore be used to study other neuronal tissues of the central nervous system. This would help researchers better understand neurodegenerative diseases, including blinding retinal diseases such as age-related macular degeneration.
In addition, potential therapies will be able to be tested on functional human ocular cells, making it possible to accelerate the development of treatments, without the use of laboratory animals. Indeed, Frans Vinberg points out that this approach can reduce research costs compared to work on non-human primates and reliance on animal models, producing results that do not always apply to humans. For example, although mice are commonly used in vision research, they don’t have a macula, unlike us.
Furthermore, Ann Hanneken says that these discoveries will certainly help to produce viable patches of human retinal tissue to treat blinding diseases. She explains : » Until now, it has not been possible to make the cells of all the different layers of the central retina communicate with each other as they normally do in a living retina. In the future, we may use this approach to develop treatments to improve vision and light signaling in eyes with macular diseases, such as age-related macular degeneration. « .
Finally, this study joins a scientific corpus on the irreversible nature or not of death. In 2018, researchers at Yale University succeeded in « reviving » a pig’s brain, 4 hours after its death, without however being able to restore overall neuronal activity. The procedure had followed the same operating scheme, that is to say the restoration of blood circulation, allowing the supply of oxygen and essential nutrients. The data collected by Abbas et al. could provide valuable keys to understanding future experiments post mortem.